As chemo cycle 3 loomed, I began to sleep less and worry more, until I came to a stunning realisation: I don’t like chemo. As revelations go, it’s not up there with Archimedes or Newton’s; it was designed to be a medical treatment, not a barrel of laughs, but thus far I had been steadfastly maintaining that worse things happen at sea. It’s still true really. In fact, worse things happen at sea to Tom Hanks alone. That poor bloke has been marooned on a desert island, chinned by pirates, and has his heart broken by mythical inhabitants of it.
It’s not so much the actual chemotherapy itself; it doesn’t hurt or anything, it’s a similar level of annoyance to having a cold. But if someone asked you if you wanted to catch a cold tomorrow, you’d probably rather not. What was bugging me more were the bits round the edges, namely the uncertainty and the impersonal nature of it all.
During radiotherapy, I had had an appointment with one of the Neuro Oncology nurses, or Paula the Oncologist every week to discuss treatment and side effects and answer any questions. This stops when radiotherapy stops. Of course there are still appointments every three months or so, and the nurses are available on the phone, so I’m still very well looked after, but there’s still a bit of a feeling of abandonment, not knowing what’s going on and not wanting to bother people with daft or unnecessary questions.
So as cycle 3 approached, I did not know what happen given the mild allergy I’d had to the Procarbazine element of PCV chemo. Would the P be removed? reduced? some other action taken? just risk taking it and see what happens? If any change to the composition of the chemo mix was made, would it still be as effective? Would the side effects increase as much as they did last time?
It wasn’t until I was actually in the day unit, having the drip for the third cycle lined up that some of these questions were answered, which brings me to my other point, about the impersonal nature of chemotherapy. At each appointment, and any trips in to the Supportive Therapies Unit, a nurse runs through a checklist of symptoms and things to watch out for. Most are perfectly innocuous – any dizziness, any nausea? But given that this is all done in an open environment, where you’re literally elbow to elbow with the next patient, it gets quite embarrassing when you’re asked to describe the consistency of your bowel movements and certain other symptoms. Maybe I’m exceptionally prudish, but that makes me uncomfortable. Poo is funny because it’s rude. I don’t want to sit in a room full of strangers and announce to them where I’m sitting on the Bristol Scale. Yes we’re all in the same boat, but still.
Worse, the doctors sometimes forget that private rooms available on the unit when they have to tell someone the worst. Sitting in STU one evening, a doctor told a lady in front of everyone that her cancer had spread to her bones, chemo would no longer be useful but they would do everything they could to alleviate any pain. Even as I and the other patients in the room bored holes in to our phones and books with our eyes, trying to avoid staring and give the lady some privacy that was lacking, I recognised her reaction. The news slid off her like a fried egg off teflon. “Bones? No, it’s my lungs! No need for pain killers doctor, I’m not in any pain!” He explained again, louder this time. She replied again that she was in no pain. Maybe the lady was not bothered – certainly her companion immediately called 3 different people to loudly relay the news. “Yes, yes, it’s bad news. It’s spread. Nothing more they can do!” Echoed each time by the lady faintly muttering that she wasn’t in any pain and was a bit confused as to why everyone thought she was. It was really quite shocking to see all this played out in front of a large room of people with not even the curtains drawn to protect her privacy, especially when there were several rooms the doctor could have taken the lady and her companion to tell them this.
So, back to the Procarbazine. I asked the chemo nurse whether it would be included this time. She confirmed it was in the package sent up by the pharmacy, but went to check with the registrar. The registrar, Shay (she’s Chinese, so this is almost certainly not how you spell her name. Sorry Shay) decided we should proceed, but with the addition of anti-histamines, hydrocortisone and E45 cream for any itching.
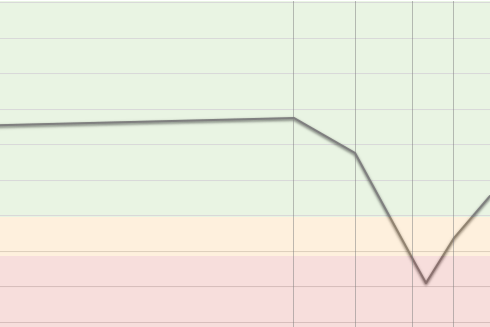
However, at this point, a new problem reared its head. Chemo kills cells that divide quickly. Unfortunately this can include things like blood cells as well as cancer cells. Platelets are the part of your blood that make it clot if you cut yourself. If your platelet levels are very low (thrombocytopenia), it can lead to cuts taking a long time to heal, spontaneous bruising and a rash called petechiae, which look like purple pinpricks. It’s nowhere near as bad as a very low white blood cell count (neutropenia), which leaves you open to serious risks from infection, but there is a threshold below which chemotherapy cannot be administered.
The normal range for platelets in the blood is 150-450 10*9/L. Mine usually hover around 290, bang in the middle of the normal range. After the first cycle of PCV, they were a creditable 238. The latest result was 81. You can’t have chemo if they’re below 95. The nurse thought this might be just a duff result, and another quick test would be in order as “I can see The Analyser is here”. It turns out The Analyser is a machine operated by a person, but I really wanted it to be a human/machine hybrid, like The Terminator, who can look at you and see all numbers showing your blood counts in its field of vision. The Analyser duly decreed that the result was not a duff. My platelets had fallen further overnight to 75.
Shay came back over, and said we would need to delay for a week, give me time to generate some more platelets. I wondered if it was the flu that had made the difference, or if there was anything I could do or avoid doing or eat or avoid eating to generate some more platelets. The answer was a resounding no to both. It’s just one of those things, and you just need to wait. Unlike a low red or white blood cell count, you can’t help it along with a transfusion or injection (unless you’re at a dangerously low, risk of spontaneous internal bleeding level). If, after a week my platelets were over 95 we could continue with PCV, but perhaps at a reduced dose, or without the Procarbazine and lower doses of the other two drugs. All of a sudden, faced with the prospect of a weaker, or no treatment, I liked chemo again. On the one hand, risking bleeding too much meant this was the closest I was ever going to get to being 19th Century inbred European royalty, but on the other hand, they all carked it and had weird chins too.
I’m rambling now, so I’ll leave the rest of the platelet saga for another time. Please don’t worry, it all works out fine in the end, but at this stage all I could do was head home for a week’s rest with two bath-sized vats of E45 cream.
I’m really glad you put that last paragraph in!
LikeLiked by 1 person
ha! Yes, I’ve learned my lesson not to leave people hanging.
LikeLike
Yes I was also relieved to hear things work out ok. You’re doing amazingly well Ruth. Quite shocked to hear about the lack of privacy. Do you think they realise how embarrassing it is for patients or is it just so run of the mill for them that it doesn’t occur to them?
LikeLike
It seems to be the latter, Jackie. They’ve seen/heard it all and it’s a very busy unit. Everyone is very caring and lovely, I guess it’s just we’ve all got different levels of comfort with talking about stuff like that in front of others.
LikeLike
My husband is having chemotherapy in Portsmouth. Private details are never talked about in front of other patients. An appointment with the doctor is made two days before each session, when all these issues are discussed, and the lady would not have got as far as chemo day before being told that bad news. It seems your hospital could learn from Portsmouth. Wishing you all the best for your treatment.
LikeLike
You’re right Elsie! To be fair, I don’t really know the context – the lady appeared to be there for a scan rather then chemo, but it’s not good. Wishing your husband all the very best too – hope he’s doing OK.
LikeLike
I’m glad your platelets did rise to the occasion in the end.
Do people tell them about the privacy thing? I complained when I went to the gestational diabetes clinic and staff were shouting women’s weight across the room (which is minor in the scheme of things) and PALS sorted that out for at least a month…
Snogs etc.
LikeLike
Good idea. I don’t think it’s worth getting PALS involved for the checklist, if it had to be done privately, it’d mean rearranging the whole unit in a way that meant far fewer people could be seen, but if I overhear anything like that lady being told she was dying again, I will talk to PALS.
LikeLike